Introduction to Kidney Diseases
Kidney diseases refer to a variety of conditions affecting the kidneys, which are crucial organs in the human body. The kidneys are responsible for several vital functions that maintain overall health and homeostasis. Primarily, they filter waste products and excess fluids from the blood, producing urine. This filtration process is essential for removing toxins and ensuring that essential nutrients and minerals remain in the bloodstream.
Additionally, kidneys play a significant role in balancing the body’s fluid levels. They regulate the volume of blood circulating in the body, maintaining proper hydration and electrolyte levels. Furthermore, kidneys assist in controlling blood pressure by managing the volume of fluids and secreting hormones such as renin, which influences blood vessel dilation and constriction.
Good kidney health is foundational for overall well-being. When the kidneys function optimally, the body efficiently eliminates waste, regulates fluids, and maintains a stable internal environment. However, when kidneys begin to malfunction, it can lead to a buildup of waste products and fluid imbalances. This can cause serious health issues, including hypertension, anemia, bone disease, and, in severe cases, kidney failure.
Understanding the various types of kidney diseases, their causes, symptoms, and potential treatments is vital for early detection and management. By recognizing the importance of these organs and the need for proactive kidney care, individuals can take steps to maintain their health and prevent the progression of kidney-related conditions.
Common Types of Kidney Diseases
Kidney diseases encompass a wide array of conditions that impact renal function. One prevalent type is chronic kidney disease (CKD). CKD is characterized by the gradual loss of kidney function over time, often caused by diabetes and hypertension. This slow progression can lead to the accumulation of waste products and excess fluids in the body, manifesting through symptoms such as fatigue, swelling, and difficulty concentrating.
Acute kidney injury (AKI), previously referred to as acute renal failure, is another significant type. AKI occurs suddenly, often due to a sharp reduction in renal blood flow, which might be a result of severe dehydration, blood loss, or sepsis. The hallmark of AKI is its rapid onset and the potential for prompt recovery with appropriate treatment, unlike the persistent progression observed in CKD.
Glomerulonephritis is an inflammatory condition affecting the glomeruli, the tiny filtering units within the kidneys. This type of kidney disease can be acute or chronic. The acute form might follow infections such as strep throat, while chronic glomerulonephritis could be linked to immune system disorders. Common symptoms include hematuria (blood in urine), proteinuria (excess protein in urine), and edema (swelling).
Polycystic kidney disease (PKD) is a genetic disorder characterized by the development of numerous cysts within the kidneys. These fluid-filled sacs can eventually impair the kidneys’ ability to function correctly. Patients with PKD often suffer from enlarged kidneys, and it’s not uncommon for this disease to be accompanied by hypertension and renal failure. Early symptoms might include flank pain, urinary tract infections, and blood in the urine.
Lastly, kidney stones are a common and often painful kidney condition. These hard deposits form from crystallized minerals and salts. They can cause severe pain, blood in the urine, and frequent urination. Depending on their size, kidney stones might pass naturally or require medical intervention, such as lithotripsy or surgical removal.
Understanding these kidney diseases, their manifestations, and distinguishing features is crucial in identifying and seeking timely medical intervention, enhancing treatment outcomes and quality of life.
Causes and Risk Factors
Kidney diseases often stem from a variety of causes, with the most notable being diabetes and high blood pressure. These conditions exert considerable strain on the kidneys over time, resulting in damage to the delicate filtering units within the kidneys, known as nephrons. In individuals with diabetes, persistently high blood sugar levels can cause these nephrons to become clogged and scarred, ultimately impairing kidney function. Similarly, high blood pressure forces the kidneys to work harder than normal, which can lead to nephrons being weakened and destroyed.
Genetic factors also play a significant role in the onset of kidney diseases. Conditions such as polycystic kidney disease (PKD) are hereditary and cause cysts to form in the kidneys, leading to impaired function and subsequent kidney failure if untreated. Family history of chronic kidney disease (CKD) can elevate an individual’s risk, highlighting the importance of awareness and regular monitoring.
Beyond these primary causes, several other risk factors can contribute to the development and progression of kidney diseases. Obesity has been closely linked with an increased risk of both diabetes and hypertension, thereby indirectly boosting the likelihood of kidney disease. Smoking, another modifiable risk factor, exacerbates kidney damage by reducing blood flow to the kidneys and accelerating the loss of kidney function.
It is imperative to consider lifestyle choices as additional risk factors. Unhealthy diets, characterized by high sodium and low nutrient intake, can elevate blood pressure and stress the kidneys. Similarly, a sedentary lifestyle contributes to the development of obesity and hypertension, precipitating kidney disease. Certain medications and supplements, when used improperly, can also cause kidney damage, particularly if taken in high doses over extended periods.
Understanding these causes and risk factors is critical in preventing the onset and mitigating the progression of kidney diseases. Regular health screenings, maintaining a healthy lifestyle, and managing existing health conditions can greatly reduce the risk and aid in the early detection of potential kidney issues.
Symptoms and Early Warning Signs
Recognizing the symptoms and early warning signs of kidney diseases is crucial for timely intervention and effective management. Kidney diseases often manifest with a range of symptoms, which may initially be subtle but can progressively worsen if left unaddressed. One of the most common symptoms is fatigue. This constant feeling of tiredness results from the kidneys’ diminished ability to remove waste from the blood, leading to an accumulation of toxins.
Another prevalent symptom is swelling or edema, particularly in the legs and ankles. This swelling occurs because the kidneys, when impaired, cannot adequately filter and expel excess fluid from the body. Consequently, fluid retention becomes evident in the extremities, causing noticeable swelling.
Changes in urination patterns are also significant indicators of potential kidney problems. Individuals may observe an increase or decrease in urine output, the presence of blood in the urine, or urine that is foamy or bubbly. Additionally, nocturia, or frequent urination at night, can be an early sign of kidney dysfunction.
Nausea and vomiting, loss of appetite, and unexplained weight loss are other symptoms that may surface as kidney disease progresses. These gastrointestinal issues result from the buildup of waste products in the body, which can negatively affect the digestive system.
Moreover, individuals may experience shortness of breath and chest pain, particularly during physical activity. These symptoms arise because fluid can build up in the lungs when the kidneys fail to function properly, exerting additional pressure on the cardiovascular system.
Recognizing these early warning signs is essential for preventing severe kidney damage. Early intervention, through medical evaluation and treatment, can help manage the disease effectively and improve the overall prognosis. Therefore, individuals experiencing any of these symptoms should seek medical advice promptly to ensure a comprehensive assessment and timely initiation of appropriate treatment options.
Diagnosis of Kidney Diseases
Diagnosing kidney diseases involves a comprehensive assessment using various medical tests to evaluate kidney function and health. Blood tests are vital in this diagnostic process, primarily focusing on levels of substances such as creatinine and blood urea nitrogen (BUN). Elevated levels of these substances can indicate impaired kidney function. The Glomerular Filtration Rate (GFR), calculated from blood creatinine levels, is another crucial measure that helps determine the stage of kidney disease.
Urine tests are also essential for diagnosing kidney conditions. A urinalysis can detect abnormal presence of protein, blood, or other substances in the urine that may signal kidney dysfunction. Furthermore, urine tests can identify bacterial infections, kidney stones, and other related disorders. A more specific urine test, the albumin-to-creatinine ratio (ACR), measures protein levels in the urine, which is critical in diagnosing chronic kidney disease.
Imaging tests such as ultrasounds and CT scans provide visual insights into the kidney’s structure and size. An ultrasound uses sound waves to create images, allowing doctors to detect abnormalities like cysts, tumors, or obstructions. CT scans, on the other hand, offer a more detailed cross-sectional view of the kidney, revealing finer details that are crucial in diagnosing more complex conditions.
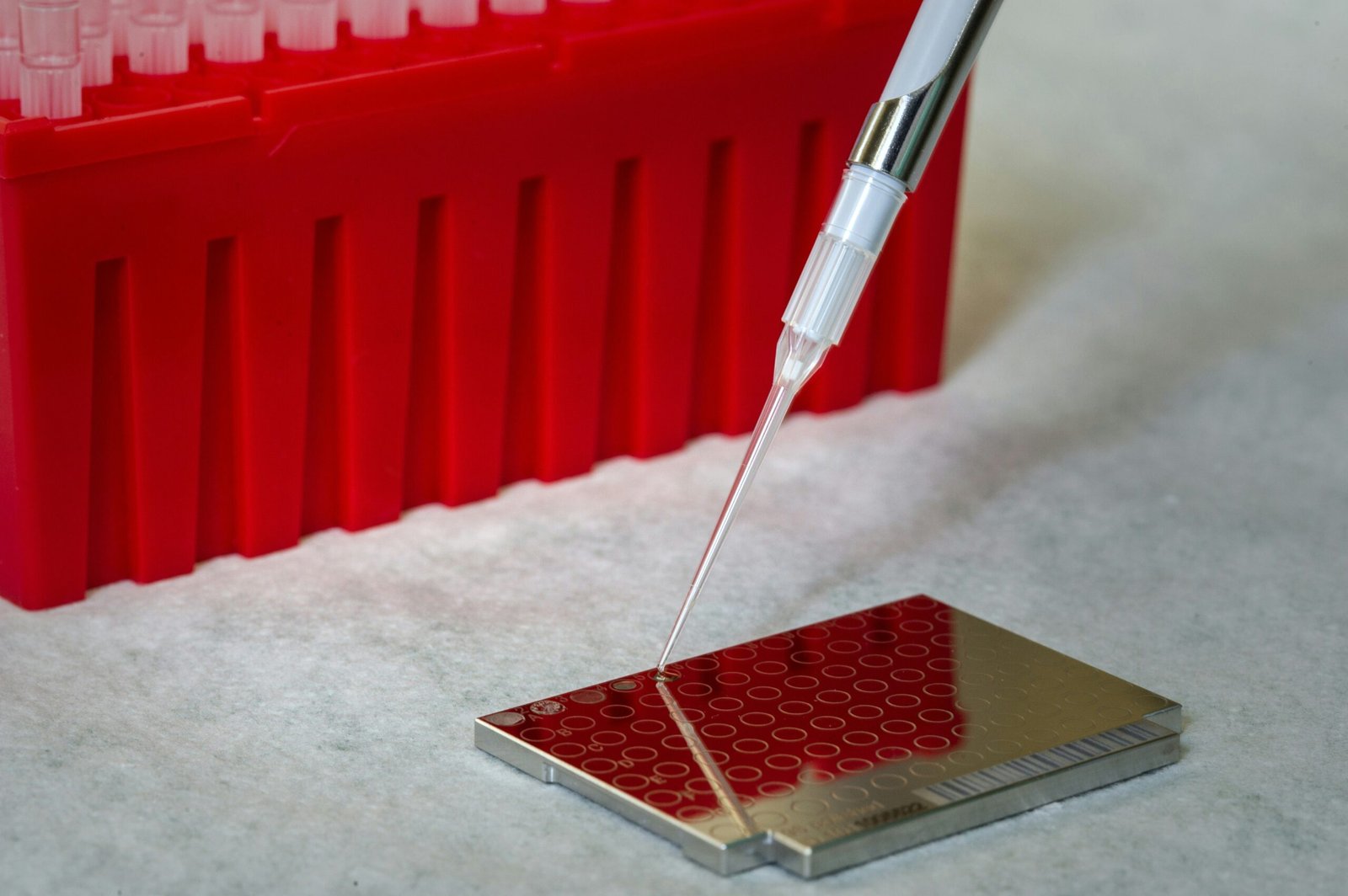
In certain scenarios, a kidney biopsy might be necessary to obtain a definitive diagnosis. This procedure involves extracting a small tissue sample from the kidney, usually performed under local anesthesia, which is then examined under a microscope. A biopsy can reveal specific details about kidney inflammation, scarring, and other abnormalities that are not apparent through blood or urine tests alone.
These diagnostic procedures collectively provide a comprehensive picture of kidney health, enabling healthcare providers to diagnose various kidney-related conditions accurately. Early and precise diagnosis is critical in managing and treating kidney diseases effectively, emphasizing the importance of these diagnostic tools.
Treatment Options
When it comes to managing kidney diseases, a variety of treatment options are available, tailored to the specific type and stage of the disease. The initial approach often involves lifestyle modifications, which are essential in controlling the progression of kidney conditions. These changes may include maintaining a balanced diet low in sodium and protein, regular exercise, quitting smoking, and limiting alcohol intake. Patients are also advised to manage their blood pressure and blood sugar levels meticulously, as these factors play a crucial role in kidney health.
Medications are another cornerstone in the treatment of kidney diseases. Depending on the individual’s condition, doctors may prescribe drugs to lower blood pressure, control blood glucose, or reduce cholesterol levels. Additionally, medications that prevent the buildup of waste products in the bloodstream or those that address underlying conditions, such as autoimmune diseases, are frequently used. It’s imperative for patients to adhere to their prescribed medication regimen to avert further kidney damage.
In advanced stages of kidney disease, more intensive treatments may be necessary. Dialysis is one such option, involving the mechanical filtering of the blood to remove toxins and excess fluids. There are two main types of dialysis: hemodialysis and peritoneal dialysis. Hemodialysis is typically performed in a medical facility, whereas peritoneal dialysis can often be done at home, offering patients more flexibility.
For some individuals, a kidney transplant may be the best course of action. This involves replacing the diseased kidney with a healthy one from a donor. Kidney transplantation can significantly improve the quality of life and longevity for those suffering from end-stage renal disease. However, the availability of donor organs and the suitability of the patient for surgery are critical determinants of this treatment option.
The choice of treatment depends heavily on the specific circumstances surrounding the patient’s condition, including the type and stage of the kidney disease, overall health, and the presence of other medical issues. A comprehensive evaluation by a healthcare provider is essential to determine the most appropriate treatment plan.
Preventive Measures and Lifestyle Modifications
Preventive measures and lifestyle modifications are crucial in maintaining optimal kidney health. One of the primary strategies involves adhering to a healthy diet. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can significantly reduce the risk of kidney diseases. It’s essential to limit the intake of salt and processed foods, which can exacerbate kidney conditions due to high sodium content and other harmful additives.
Regular physical activity is equally important. Engaging in exercises such as walking, cycling, or swimming for at least 30 minutes most days of the week helps improve cardiovascular health, reduce blood pressure, and manage weight. These benefits collectively support kidney function and reduce the risk of developing conditions like hypertension and diabetes, which are common precursors to kidney diseases.
Staying hydrated is another vital component of kidney health. Drinking adequate amounts of water facilitates the removal of waste products and toxins from the blood through urine. It’s generally recommended to consume at least 8 glasses of water per day, although individual needs may vary based on factors such as activity level, climate, and overall health.
It is also imperative to manage underlying health conditions diligently. Diabetes and hypertension are among the leading causes of kidney damage. Regular monitoring of blood sugar levels and blood pressure, along with appropriate medical treatments, can help mitigate their adverse effects on the kidneys. Patients with these conditions should work closely with their healthcare providers to develop and adhere to a comprehensive management plan.
Lastly, avoiding smoking and limiting alcohol consumption can have a positive impact on kidney health. Smoking restricts blood flow to the kidneys, leading to diminished function, while excessive alcohol intake can lead to dehydration and increased blood pressure. Lifestyle changes geared towards these preventive measures can profoundly enhance kidney health and overall well-being.
Living with Kidney Disease: Tips and Support
Living with kidney disease presents numerous emotional and physical challenges that require a comprehensive approach to care. Patients must navigate a landscape of medical appointments, dietary restrictions, and emotional stress. Acceptance of the disease is fundamental, but learning to manage living with kidney disease can significantly improve one’s quality of life.
One crucial aspect of managing kidney disease is adhering to treatment plans prescribed by healthcare professionals. These plans often include medications, dietary restrictions like reducing salt and protein intake, and regular monitoring of kidney function. Following these recommendations closely can help slow the progression of kidney disease and prevent complications. Make use of reminders and organizational tools to stay on track with appointments and medications.
Coping with the emotional ramifications of kidney disease is equally important. Feelings of frustration, anxiety, and depression are common among patients. Engaging in activities that promote mental well-being, such as exercise, meditation, and hobbies can be beneficial. Additionally, talking to a mental health professional can provide strategies to manage emotional stresses effectively.
Another critical element for individuals living with kidney disease is finding a robust support network. Support can come from various sources, including healthcare providers, family, friends, and dedicated support groups. Healthcare providers can offer valuable guidance and answer any questions related to the disease and its management. Family and friends can provide emotional support and assistance with daily tasks, alleviating some of the burdens of the disease.
Support groups, both in-person and online, offer a unique space for patients to share their experiences and strategies for coping with kidney disease. These groups can provide emotional reassurance and practical advice, fostering a sense of community among individuals facing similar challenges.
In navigating the complexities of kidney disease, having access to patient resources is vital. These resources can include educational materials, community programs, and online forums managed by healthcare organizations. They provide valuable information, helping patients stay informed about their condition and any new treatment options available.