Introduction to Antibiotics
Antibiotics are a class of drugs used to combat bacterial infections. Since their discovery, they have played an indispensable role in modern medicine, radically transforming healthcare by providing effective treatments for numerous bacterial diseases. The first antibiotic, penicillin, was discovered by Alexander Fleming in 1928. This groundbreaking discovery heralded a new era in medical science, making it possible to treat previously deadly infections with unprecedented efficacy.
The Discovery of Penicillin
Alexander Fleming’s discovery of penicillin was a turning point in medical history. Prior to this, bacterial infections were often fatal, with limited treatment options available. Fleming’s observation of the mold Penicillium notatum led to the development of penicillin, the first true antibiotic. This groundbreaking discovery enabled doctors to treat infections such as pneumonia, strep throat, and syphilis with remarkable success. The advent of penicillin set the stage for the development of other antibiotics, each targeting different types of bacteria.
The Impact of Antibiotics on Modern Medicine
Antibiotics have transformed healthcare, addressing deadly diseases and supporting advanced medical procedures. They are crucial for treating infections and enabling complex treatments like surgery and chemotherapy.
How Antibiotics Function
Antibiotics combat bacteria by either killing them or preventing their growth. This allows the immune system to remove the remaining bacteria and promote recovery. They are used to treat various infections, such as those affecting the respiratory system, urinary tract, and skin. Their broad applications make them vital for managing both common and serious conditions.
Historical Impact of Antibiotics
Before antibiotics, even minor infections could be life-threatening. Their introduction drastically reduced death rates and improved overall quality of life. Recognizing their historical impact highlights their importance in today’s healthcare landscape.
Types of Antibiotics and Their Uses
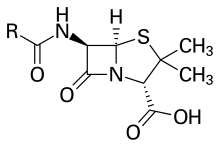
Beta-Lactams
Beta-lactams, including penicillins and cephalosporins, are essential antibiotics. Penicillins target Streptococcus infections, while cephalosporins are used for a range of infections like urinary tract and skin infections.
Macrolides
Macrolides, such as erythromycin and azithromycin, inhibit bacterial protein synthesis. They are effective for treating respiratory infections, sexually transmitted infections, and certain skin conditions.
Tetracyclines
Tetracyclines, like doxycycline, inhibit bacterial growth. They are useful against acne, chlamydia, and some forms of pneumonia.
Aminoglycosides
Aminoglycosides, including gentamicin and tobramycin, are reserved for severe infections such as sepsis. They work by disrupting bacterial protein synthesis but can be toxic.
Fluoroquinolones
Fluoroquinolones, such as ciprofloxacin and levofloxacin, are broad-spectrum antibiotics. They treat a wide variety of infections, including urinary tract and gastrointestinal infections, by interfering with bacterial DNA replication.
Selecting the appropriate antibiotic is key to effective treatment and minimizing resistance. Misuse or overuse can lead to resistant strains, complicating treatment.
Antibiotic Resistance: Causes and Consequences
Antibiotic resistance is a serious global health issue. It arises when bacteria develop ways to resist the effects of drugs meant to kill them. Resistance can occur through genetic changes or gene acquisition from other bacteria, allowing these resistant strains to spread and reduce drug effectiveness.
Overuse and Misuse
The overuse and misuse of antibiotics significantly contribute to resistance. Patients often misuse antibiotics by not completing their prescriptions or using them for viral infections, where they are ineffective. Additionally, antibiotics used in agriculture for growth promotion can also promote resistance.
Lack of New Antibiotics
The shortage of new antibiotics exacerbates the resistance problem. Pharmaceutical companies focus more on chronic disease medications, resulting in fewer new antibiotics being developed.
Global Health Implications
Antibiotic resistance poses severe risks. We may face a return to a pre-antibiotic era where manageable infections become deadly. For instance, drug-resistant tuberculosis causes about 240,000 deaths annually, while methicillin-resistant Staphylococcus aureus (MRSA) presents significant treatment challenges. By 2050, resistance could result in up to 10 million deaths per year.
Real-World Examples
In India, antibiotic-resistant infections in neonates cause over 58,000 deaths each year. The global spread of resistant bacteria underscores the urgent need for effective antimicrobial stewardship and ongoing research.
The Future of Antibiotics and Alternative Strategies
Bacteriophage Therapy
Research into alternative treatments is promising. Bacteriophage therapy uses viruses that target specific bacteria, offering a precise method to address infections while preserving the natural microbiome.
Antimicrobial Peptides (AMPs)
Antimicrobial peptides (AMPs) are another promising avenue. These natural molecules have strong antibacterial properties and may lead to new antibiotic formulations. They typically work by disrupting bacterial cell membranes, which can reduce the likelihood of resistance.
CRISPR Technology
CRISPR technology offers potential for future antimicrobial strategies. By editing genes responsible for antibiotic resistance, scientists can enhance the effectiveness of existing antibiotics.
Global Cooperation
Addressing antibiotic resistance requires global collaboration. Sharing research and resources internationally can improve strategies to combat resistance. Regulatory policies and education are essential for promoting responsible antibiotic use.
Individual Actions
Patients should adhere to prescribed antibiotic courses and avoid using antibiotics for viral infections. These practices help prevent resistance and ensure the continued effectiveness of antibiotics.
By combining global efforts and innovative research, we can ensure the future effectiveness of antibiotics and maintain effective treatments for future generations.


Comments